Cobb angle is the “universal standard” of measurement used to quantify a scoliosis for the purpose of measuring curve progression over time. Evaluating scoliosis via Cobb angle is important since it is often the first objective indicator. A curve is considered to be scoliosis at a Cobb angle of 10º or more. Any increase greater than 5º or 10º is considered a change – the number varies among studies, however 5º is the accepted measurement according to most physicians. Scoliosis is considered mild at 10º-24º, moderate at 25º-50º and severe at >50º depending on the source.
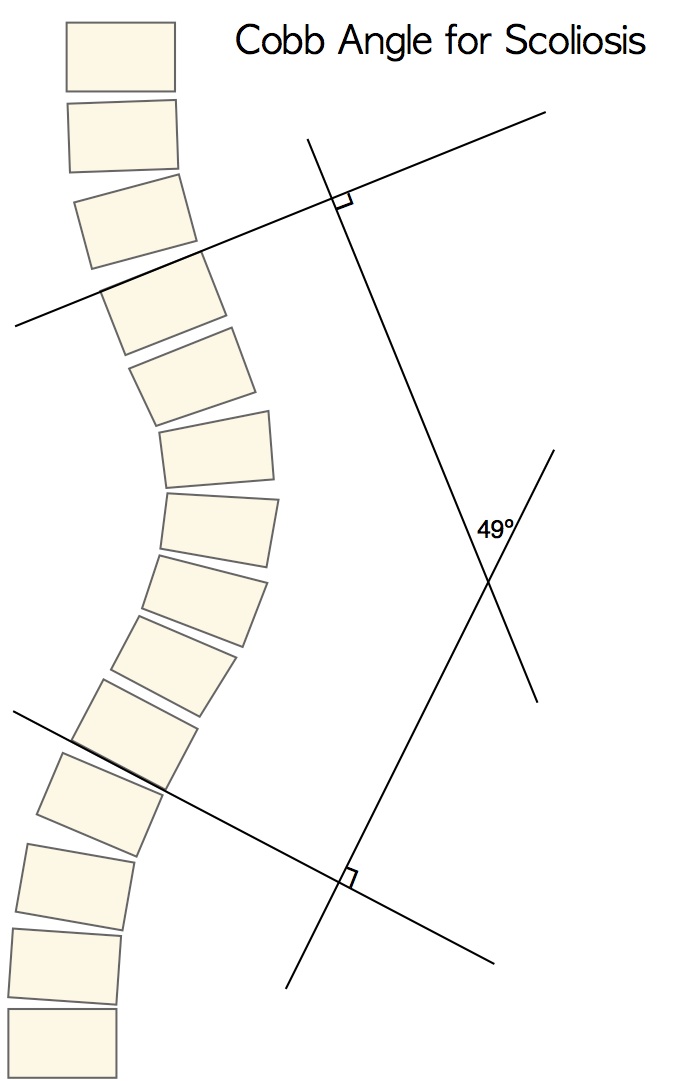
Cobb angle is measured on a ‘PA’ (posterior-anterior or back to front) x-ray as follows: A line is drawn at the top of the vertebra (above the curve apex) with the greatest lateral tilt and another line is drawn at the bottom of the vertebra (beneath the curve apex) with the greatest lateral tilt. The lines should be extended into the margin of the film. Next, third and fourth perpendicular lines are drawn. The angle is calculated where the lines intersect.
While Cobb angle is an important measurement, it is only one piece of the pie and not without limitations. One shortcoming is that measurements often vary from doctor to doctor because human judgment is involved in choosing which vertebrae are most tilted. Another is that the Cobb angle is a two-dimensional view of a three-dimensional condition. So Cobb angle alone does not fully capture the complexity of a scoliotic curve.
Awareness of additional idiosyncrasies of Cobb’s angle can also be helpful for parents and patients. For instance, when undergoing x-rays for scoliosis the patient should make every effort to ensure as many factors as possible are constant. In particular, obtain x-ray readings at the same time of day due to reported variations in intraday measurements, reportedly as great as 20º (Beauchamp et al 1993). Furthermore, the patient should assume the same position in each x-ray series. If the initial X-ray is standing then subsequent X-rays should also be standing. Posture also affects Cobb angle measurement. The patient should avoid slouching and stand exactly the same way during each subsequent x-ray.
To determine flexibility vs. rigidity, there is an advantage to having X-rays taken both standing and supine on the same day and time. Knowledge of spinal flexibility or rigidity is useful for the Schroth practitioner or the practitioner fitting a brace. For example, if the standing x-ray Cobb angle is 40º and the supine x-ray Cobb angle is 20º this indicates some degree of spinal flexibility. On the other hand, if there is no change in Cobb angle degree when X-rays are taken in a standing and supine position on the same day, the spine is considered rigid. In this case, it is less likely a significant correction will be able to be achieved. Conversely, if the Cobb angle measurement indicates that there is flexibility, some degree of correction may be expected in a corrective brace, or from Schroth curve-pattern specific scoliosis exercises.
Patients and parents can get overly focused on the Cobb angle measurement. Of course, it is understandable and easy to do when you are the parent of a child, or a patient, with scoliosis. Perhaps, one reason for this is that spinal surgeons frequently reference a 45-50º Cobb angle as the degree where surgical intervention for scoliosis is recommended. By the way, this threshold is a point of contention between advocates of conservative care and spinal surgeons and even surgeons have different opinions on this, some being more conservative than others.
Despite its shortcomings, to the Schroth method practitioner, the Cobb angle is an important measurement. In the case of mild scoliosis in particular, the Cobb angle is an indicator for parents of adolescents to become proactive rather than choosing to observe what may happen.
In addition to Cobb angle, at Scoliosis 3DC® we include additional assessments for a more comprehensive evaluation of a scoliosis of any degree. These include Scoliometer™ readings, lung capacity and chest expansion measurements. Of course, cosmetic factors such as rib prominence and postural imbalances are not measurable by Cobb’s angle and these are of utmost importance.
Evaluation using various measures allows the Schroth practitioner to gain a better understanding of each curve and its effects on rib mobility and pulmonary function. These will be addressed independently in future blogs as part of this continuing series.
Coming soon: Evaluating Scoliosis-Part 2-Scoliometer Reading

