Risser 4 indicates ossification of the iliac crest apophysis at 75% or more. “Capping” from lateral to medial (outside to inside) is nearly complete and skeletal maturity is approaching. From our perspective, there is more to say about Risser 4 than the other Risser stages. This is due to our use of different management techniques, braces and objectives for patient care compared to traditional medical establishment protocols.
If you follow our blogs, you know we advocate conservative treatment for adolescent idiopathic scoliosis (AIS) as early as possible after a diagnosis. Unfortunately, not every patient has that opportunity. Parents of Risser 4s usually tend to seek out our treatment approach after a late diagnosis or when progression has occurred after following questionable advice, brace failure, or being told, “your child needs scoliosis surgery.”
But, is surgery really necessary? That’s an individual decision. Is Risser 4 too late to treat? The fact is, at Risser 3 or 4, there are some patients with spinal flexibility and the opportunity for residual growth, enough to suggest that radiological and postural improvements can be made. It’s not always easy to know which patients these might be. Certainly, not all of our successful patients can be outliers though! Isn’t trying to improve the spine before the completion of growth worth a try?
With any type of scoliosis treatment, outcome is difficult to predict for a given individual, despite the Risser stage. However, with pattern-specific-scoliosis rehabilitation (PSSR), with or without bracing, nearly all of our patients have demonstrated at least some type of improvement (ie. better posture, decreased rotation, more balanced shoulders or pelvis, improved pulmonary function, reduced Cobb angle measurement etc.)–even when treatment doesn’t begin until the later stages of growth.
It’s safe to say the majority of surgeons would disagree with our position. If you were to ask a surgeon about bracing at Risser 4, most will dismiss it. Several patients have come to us for a brace who have been denied bracing. They’ve been told that surgery is the only answer. Others have been told to “watch and wait” at that point to see if surgery will be necessary. The treating establishment operates under the premise that “a Risser sign of 4 correlates with the cessation of spinal growth” (1). As a result, it’s common for surgeons to recommend brace weaning, especially for girls, at Risser 4. It was the benchmark used for weaning in BrAIST (2).
To this point, Dr. Marc presented at the AOPA (American Orthopedic and Prosthetic Association) in Las Vegas last September. The talk addressed the question, Is Idiopathic Scoliosis ≥40° Amenable to Bracing at the Later Stages of Skeletal Maturity? His presentation included several cases of patients showing improvements, either posturally, on x-ray, or both. Included in his supporting research was a 2012 study which stated, “Clinicians should remain cognizant…that vertebral growth can persist even at Risser Stage 4” (3).
As you have surmised, we don’t view Risser 4 as the end of the road for attempting to improve scoliosis. The fact of the matter is that determining the end point of growth is complex. However, the Scoliosis 3DC® program works to take advantage of any remaining residual growth on a case-by-case basis.
We manage scoliosis via our up-to-date pattern-specific rehabilitation and compatible brace – all based on Schroth principles and classifications. The combination of the two can be very effective, but not everyone will have equal success. Even so, we feature two cases below which demonstrate that there is hope, even at the later stages of skeletal maturity. We must also give credit where credit is due – to the patients. Both have worked hard to achieve their results.
Case 1: Last year, The Open Orthopaedics Journal, published our case study of a 15-year-old girl who began treatment at Risser 4–three years post-menarche. In 2016, she elected to participate in our pattern-specific scoliosis exercise program after it was recommended she have surgery for her scoliosis. Instead, this young-lady reduced her curvature by 13º in one year using only our exercise protocols. Read more about her case, in detail, here.
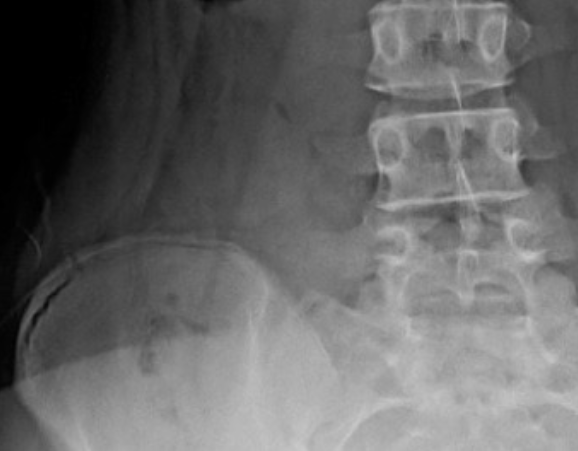
Case 2: Another Risser 4 patient, a 13-year-old girl from NY, came to see us after being recommended for surgery with curves measuring 58º and 31º at the time. Rather than consenting to surgery, her parents brought her to be fitted with a brace ASAP. She also participated in our intensive Schroth program. The patient was 20 months post-menarche. Despite all of this, her in-brace correction was an impressive 69%–indicating a flexible spine. She is now 16 years old and has been in her brace for three years– staying a Risser 4 the entire time. (An interesting tidbit about Risser 4 – sometimes a patient can remain a Risser 4 for quite a while).

Two years after her first brace, the patient’s height had increased by more than 5 centimeters, so she was fit with a second brace. Whether this was due to her excellent correction, residual growth, or a combination of the two, it doesn’t really matter. What matters is her outcome! She is now taller and straighter WITHOUT SURGERY or its risks. Her curves are now 31º and 24º (per her 24 hour out-of-brace x-ray). We know you can do math, but that’s an incredible 27º and 7º reduction. Dr. Marc suspects this patient is now nearly skeletally mature and he anticipates she will be able to wean from her brace after her next x-ray.
We are not implying every Risser 4 patient will get these results. They won’t. In fact, we caution parents and patients to approach conservative care with reasonable expectations, no matter what the Risser sign is at the time treatment starts. This is because each spine is unique and several patient-dependent factors affect outcome. Less flexible spines will have more of a challenge effecting change (especially on x-ray). It is also important to note that halted progression or no change in between follow-up x-rays should be considered a successful/positive result as historically, the role of scoliosis intervention is to prevent the curvature from getting worse.
Patient compliance also plays a role. That said, there are some patients, even compliant ones, whose outcomes are just not as impressive as others. Conversely, we’ve also had some semi-compliant patients who have still done very well. The point is, everyone is different so making predictions about individual outcomes is unwise.
(1) Lonstein, JE, et al. Moe’s Textbook Of Scoliosis And Other Spinal Deformities. 3rd ed. Philadelphia, Pa:Saunders,1995;76.
(2) Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of Bracing in Adolescents with Idiopathic Scoliosis. The New England journal of medicine. 2013;369(16):1512-1521.
(3) Hacquebord JH, Leopold SS. In Brief: The Risser Classification: A Classic Tool for the Clinician Treating Adolescent Idiopathic Scoliosis. Clinical Orthopaedics and Related Research. 2012;470(8):2335-2338.

