What is idiopathic scoliosis?
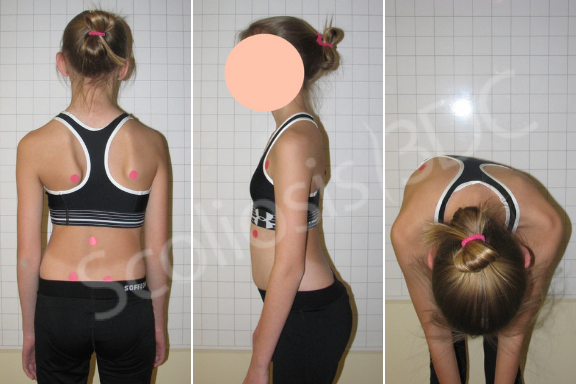
Idiopathic scoliosis (IS) is a complex 3-dimensional condition of the spine and trunk. Although many consider scoliosis to be a single spinal curve, the 3-dimensionality means that not only does the spine bend laterally but also rotates/twists in the transverse plane and may be flattened when viewed from the side. Patients with idiopathic scoliosis often present with trunk asymmetries, unlevel shoulders, and rib and/or lumbar prominences. These are most noticeable in the forward bending position (see photo). As the body tries to remain upright compensatory curves develop. According to the ALS (Augmented Lehnert-Schroth) system, the spine will decompensate into three or four curves. Education and exercise rehabilitation are recommended, especially for growing children, since the condition can worsen rapidly.
80%-90% of all scoliosis cases are considered to be idiopathic in origin. The term idiopathic means no known cause (no associated pathology and an absence of underlying neurological, muscular and/or vertebral irregularity). Although there are many theories related to the cause of idiopathic scoliosis, none are proven. Idiopathic scoliosis is divided into three subcategories: infantile (IIS), juvenile (JIS), and adolescent (AIS). Idiopathic adult scoliosis may be a continuation of scoliosis from childhood or adolescence or the result of a missed diagnosis but still idiopathic in origin. For each subcategory, there are various suggested theories of etiology.
Pain is rare in children with idiopathic scoliosis. Those experiencing pain may have a co-occurring disorder or an underlying condition that may be causing scoliosis (i.e. an injury). Based on clinical experience, discomfort near the convexity of the apex (outer most portion of the most curved part of the spine) is typically secondary to muscle fatigue and usually resolves once intervention begins. This type of discomfort does not warrant the need for an MRI. However, an MRI for scoliosis is recommended when there is significant pain, an abnormal curve pattern (i.e. left thoracic curve), neurologic deficits, unusually rapid progression, males, early-onset, and incongruous rigidity.
The natural history of IS is difficult to report concisely because many factors contribute to its stabilization or progression. In general, it is accepted that larger curves are more likely to progress; curves greater than 30º may progress in adulthood; the earlier the onset, the more likely progressive scoliosis will become severe; single thoracic curves are more likely than double curves to be progressive because body statics are less balanced; larger curves occur more often in females; sagittal plane deformity is more likely to cause pain than the lateral curvature of scoliosis; and finally, menopause and pregnancy may cause a curve to increase more than standard progression rates in adulthood.

Scoliosis can be functional or structural. Functional scoliosis occurs before there is deformity of the vertebral elements. Structural scoliosis occurs as a result of ongoing asymmetric vertebral loading, which creates a fixed spinal abnormality. Treatment which incorporates a suitable rehabilitation program may help interrupt functional scoliosis and prevent structural changes that may occur as a result of the vicious cycle of progression.
Treatment for idiopathic scoliosis
The complex nature of idiopathic scoliosis has led to the development of multiple treatment options. Knowing and understanding the condition’s natural history is crucial to selecting treatment protocols to ensure there is neither undertreatment nor overtreatment. When considering scoliosis treatment, one must take into account the constant development of medicine, variety in research, the experience level and specialization of the practitioner, and clinical reasoning for individual cases (i.e. textbook case vs. unusual case). It is important that families understand that scoliosis is unique to the individual and must be treated accordingly. Available research is valuable but must be carefully analyzed in terms of level or quality of research, significance, sample size, study strengths/weaknesses, and practitioner knowledge/experience.
Idiopathic scoliosis is a complex condition and successful treatment is not measured by curve size alone. Successful idiopathic scoliosis curve management, is based on one or more of the following: stopping progression, bringing the curve toward the midline, managing/improving postural appearance, managing pain if present, empowering the patient/caregiver, decreasing spinal rotation, improving the physiology of the sagittal plane and reducing Cobb angle(s) when possible (for children and adolescents with remaining growth). Factors that contribute to or hinder success include, but are not limited to, age, curve pattern, curve size, gender, compliance, growth velocity, curve flexibility/rigidity, functional tethering, cognition, and family support. The course of scoliosis in any particular individual cannot be reliably predicted. This is due to the multi-factorial aspects and individuality of the condition.
Scoliosis surgery for AIS is often recommended by spinal surgeons when a curve progresses to a severe Cobb angle prior to skeletal maturity (greater than 45°). However, research has concluded that quality of life, pain, and mental health are not always positively impacted by surgery. Furthermore, because of the very nature of scoliosis surgery, there is always the risk of complications and even that revision surgery may be needed at some point in the future.
Conservative treatment for idiopathic scoliosis has historically referred to bracing. Today, conservative treatment now includes pattern-specific scoliosis rehabilitation (PSSR). Scoliosis-specific exercise is designed to increase flexibility, strength, and to improve postural asymmetries. Exercises should be age and developmentally appropriate. For some kids, it can be a way to reinforce or enhance the effects of bracing.
The trend for patients with idiopathic scoliosis is shifting toward conservative treatment interventions. When we introduced the Schroth method here there were many skeptics. Today, parents and even some medical doctors are increasingly becoming more aware of the benefits of non-surgical treatment. Parents and patients are making different choices.
Still, the status quo hangs on. Here at Scoliosis 3DC®, we rarely subscribe to ‘watch and wait for patients with mild idiopathic scoliosis who are at risk for progression. We urge parents to look into starting treatment earlier rather than later. Whether the curve is mild, moderate, or severe, our goal is to educate patients and to ensure that they have all the tools to interrupt asymmetric spinal loading and the vicious cycle of progression.
Increasing availability to more advanced Schroth rehabilitation treatment protocols, newer research, and more experienced and enlightened practitioners now mean that conservative scoliosis management with exercise and 3D bracing can offer clinically significant outcomes for compliant patients. With that said, parents and patients should choose their program and practitioner carefully. Individual practitioners, practice styles, and programs can vary significantly. Lost time with the wrong program or practitioner during growth means lost potential for improvement.
Bracing for idiopathic scoliosis has changed as well. At a minimum, as always, the goal of bracing for skeletally immature adolescents and children is stabilization of the curve(s). With the advancements and improvements in asymmetric 3D scoliosis bracing from Europe some braces now work to attempt curve reduction – at least to some extent. Prescribed brace wear time will vary by child but for at-risk children and adolescents, it is often about 20 hours per day. In-brace correction is also an important factor. An experienced practitioner aims for a 30%-50% in-brace correction for adolescents, meaning curve magnitude is reduced when the brace is worn by 30%-50%. However, the closer to bone maturity the patient is the less likelihood of a 50% in-brace correction because, in general, spinal flexibility decreases as a patient grows closer to skeletal maturity. For the skeletally immature patient (a low Risser and pre-menarcheal) with a flexible spine, an in-brace correction of 30% to 50% is a reasonable expectation. For those with more spinal flexibility, a good in-brace correction can be used to the patient’s advantage during growth! With asymmetric bracing, the intent is that when it is time for brace weaning – after bone maturity (Risser 5) – the curve will settle somewhere between the pre-bracing Cobb angle and the in-brace correction measurement. Recent evidence shows that curve-specific exercises (PSSR) together with brace wear may help stabilize and improve the Cobb angle better than bracing alone. For patients and their parents who have been informed that surgery is a child’s only option, pursuing aggressive conservative treatment protocols for idiopathic scoliosis may help their children avoid that fate. Link here for Schroth method results for severe scoliosis cases treated at Scoliosis 3DC®.
To learn more please call us at 781-938-8558 or email info@scoliosis3dc.com. Among our many goals for our patients with idiopathic scoliosis is empowerment over the condition.
References:
Lonstein JE. Idiopathic Scoliosis. In: Lonstein J, Bradford D, Winter R, Ogilvie J (editors). Moe’s textbook of scoliosis and other spinal deformities. Philidelphia: WB Saunders Company 1994, pp. 219-256.
Fadzan M, Bettany-Saltikov J. Etiological theories of adolescent idiopathic scoliosis: past and present. The Open Orthopaedics Journal. 2017;11(1):1466–1489.
Hawes MC. Scoliosis and the human spine: a critical review of clinical approaches to treatment of spinal deformity in the United States, and a proposal for change. Stoughton, MA: Exclusive distributor, National Scoliosis Foundation; 2010.
Wick JM, Konze J, Alexander K, Sweeney C. Infantile and juvenile scoliosis: the crooked path to diagnosis and treatment. Aorn Journal. 2009;90(3):347–380.
Lincoln TL. Infantile idiopathic scoliosis. American Journal of Orthopedics. 2007;36(11):586–90.
Weiss HR, Lehnert-Schroth C, Moramarco M, Moramarco K. Schroth Therapy – Advancements in Conservative Scoliosis Treatment. Saarbrüecken: Lambert Academic Publishing (LAP) 2015.
Hawes MC, O’Brien JP. The transformation of spinal curvature into spinal deformity: pathological processes and implications for treatment. Scoliosis. 2006;1(1):3.
Stokes IAF, Burwell RG, Dangerfield PH. Biomechanical spinal growth modulation and progressive adolescent scoliosis — a test of the ‘vicious cycle’ pathogenetic hypothesis: summary of an electronic focus group debate of the IBSE. Scoliosis. 2006;1:16.
Du Q, Zhou X, Negrini S, Chen N, Yang X, Liang J, Sun K. Scoliosis epidemiology is not similar all over the world: a study from a scoliosis school screening on Chongming island (China). Bmc Musculoskeletal Disorders. 2016;17:303–303.
Trobisch P, Suess O, Schwab F. Idiopathic scoliosis. Deutsches Arzteblatt International. 2010;107(49):875–83.
Ozturk C, Karadereler S, Ornek I, Enercan M, Ganiyusufoglu K, Hamzaoglu A. The role of routine magnetic resonance imaging in the preoperative evaluation of adolescent idiopathic scoliosis. International Orthopaedics. 2010;34(4):543–546.
Asher MA, Burton DC. Adolescent idiopathic scoliosis: natural history and long-term treatment effects. Scoliosis. 2006;1(1):2.
James JIP. Idiopathic scoliosis. The Journal of Bone and Joint Surgery Br. 1954;36:36–49.
Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy J-PC, Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002;27(4):387–392.
Marty-Poumarat C, Scattin L, Marpeau M, Garreau de Loubresse C, Aegerter P. Natural history of progressive adult scoliosis. Spine. 2007;32(11):1227–1234.
Marty-Poumarat C, Ostertag A, Baudoin C, Marpeau M, de Vernejoul MC, Cohen-Solal M. Does hormone replacement therapy prevent lateral rotatory spondylolisthesis in postmenopausal women? European Spine Journal. 2012;21(6):1127–1134.
Dewan MC, Mummareddy N, Bonfield C. The influence of pregnancy on women with adolescent idiopathic scoliosis. European Spine Journal. 2018;27(2):253–263.
Weiss HR, Negrini S, Rigo M, Kotwicki T, Hawes MC, Grivas TB, Maruyama T, Landauer F. Indications for conservative management of scoliosis (guidelines). Scoliosis. 2006;1:5.
Upasani VV, Caltoum C, Petcharaporn M, Bastrom TP, Pawelek JB, Betz RR, Clements DH, Lenke LG, Lowe TG, Newton PO. Adolescent idiopathic scoliosis patients report increased pain at five years compared with two years after surgical treatment. Spine. 2008;33(10):1107–12.
Ward WT, Friel NA, Kenkre TS, Brooks MM, Londino JA, Roach JW. SRS-22r scores in non-operated adolescent idiopathic scoliosis patients with curves greater than forty degrees. Spine. 2017;42(16):1233–1240.
Gluch H, Mueller F. Cotrel-dubousset instrumentation for the correction of adolescent idiopathic scoliosis. long-term results with an unexpected high revision rate. Scoliosis. 2012;7(1):13.
Weiss HR, Goodall D. Rate of complications in scoliosis surgery – a systematic review of the PubMed literature. Scoliosis. 2008;3:9.
Weiss HR, Tournavitis N, Seibel S, Kleban A. A prospective cohort study of AIS patients with 40° and more treated with a Gensingen brace (GBW): preliminary results. The Open Orthopaedics Journal. 2017;11(1):1558–1567.
Peterson LE, Nachemson AL. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from the brace study of the Scoliosis Research Society. The Journal of Bone and Joint Surgery Am. 1995;77(6):823–827.
Clin J, Aubin CÉ, Sangole A, Labelle H, Parent S. Correlation between immediate in-brace correction and biomechanical effectiveness of brace treatment in adolescent idiopathic scoliosis. Spine. 2010;35(18):1706–13.
van den Bogaart M, van Royen BJ, Haanstra TM, de Kleuver M, Faraj SSA. Predictive factors for brace treatment outcome in adolescent idiopathic scoliosis: a best-evidence synthesis. European Spine Journal. 2019;28(3):511–525.

