In 1958, Joseph C. Risser, published his findings on growth and the completion of growth in a paper entitled, “The Iliac Apophysis: An Invaluable Sign in the Management of Scoliosis.” His findings led to the Risser sign classification system used to assess skeletal maturity. While Risser sign is still used today by doctors to estimate remaining growth in adolescents, we find that many parents are still unaware of this long-used system.
At Scoliosis 3DC®, we are all about empowering families through education. This is so that parents are able to make the very best decisions for scoliosis management. How can a parent/patient hope to manage scoliosis effectively without a complete understanding of the factors that need to be considered during treatment?
For scoliosis awareness month we thought we’d provide some insights on Risser sign (also referred to as stage, classification, grade, value, score, range, etc.) in hopes of adding to your base of knowledge. Subsequent posts will feature cases we’ve treated at various Risser stages.
Risser sign represents the stage of ossification (process by which new bone is formed) of the iliac crest apophysis. Because vertebral growth plates are difficult to visualize/evaluate, Dr. Risser was looking to find an alternative for evaluating vertebral growth potential, since growth potential has tremendous significance when it comes to treating adolescent idiopathic scoliosis. Risser found that the “completed excursion and ossification of the iliac apophysis were generally concurrent with that of vertebral growth plates” and that the attachment of the iliac apophysis is an accurate indication of completed spinal growth (1).
This finding was key for practitioners treating scoliosis, as they now had another tool to classify scoliosis and make treatment recommendations according to estimated remaining growth potential (along with other factors, such as age, sex, Cobb angle, etc.). Risser sign classifications are on a scale of 0-5. Risser 0 indicates that there is a significant amount of growth remaining, while Risser 5 indicates skeletal maturity.
Doctors follow the amount of ossification on a patient’s x-ray to determine the Risser sign (pelvis must be visualized). This is best seen from an AP (anteroposterior) standing full-spine x-ray and is referred to as ‘capping.’ This capping occurs from the outside to inside of the iliac crest (see image below).
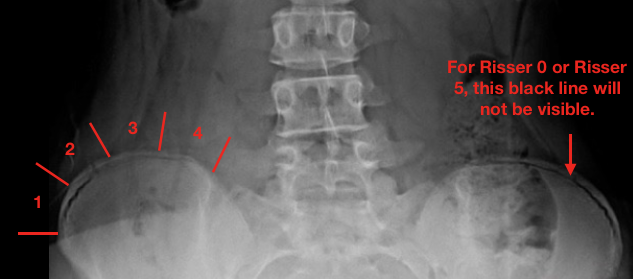
Risser 1 – approximately 25% apophysis of the iliac crest
Risser 2 – approximately 25-50% apophysis of the iliac crest
Risser 3 – approximately 50-75% apophysis of the iliac crest
Risser 4 – approximately 75% apophysis of the iliac crest
Risser 5 – complete ossification and fusion of the iliac crest apophysis
As described above, Risser signs 1-4 can be determined by the amount of capping shown while Risser 0 is when no ossification center is seen in the apophysis and Risser 5 is complete ossification. As shown above, Risser 0 and Risser 5 can sometimes appear similar, so age and long bone growth plates (such as a hand x-ray) can help to distinguish between the two. For reference, the average chronological age of iliac apophysis in girls is 14 years old. In boys, it’s 16. However, it can be earlier or later, depending on the individual. For females, menarcheal status should also be considered (pre-menarcheal females are more likely to be Risser 0 than Risser 5).
Dr. Risser had noted in a previous study that spinal column growth is slower in children between 5 and 10 years old, and faster in children between 10 and 15 years old. That said, once adolescence begins – the risk for scoliosis progression increases (2). As we post, we hope you will recognize and appreciate the benefits of treatment at the earlier stages of scoliosis and that, with the right treatment, at any stage, surgery does not always have to be the inevitability it is often presented as.
1) Risser, JC, The Iliac Apophysis: An Invaluable Sign in the Management of Scoliosis. Clin Orthop Relat Res (2010) 468(3):646–653. DOI 10.1007/s11999-009-1096-z.
2) Risser, JC, and Ferguson, AB: Scoliosis: its prognosis, J. Bone & Joint Surg. 18:667, 1936.

